On-body Injector Patient Instructions for Use:
Which version of the Instructions for Use did your doctors's office give you?
If you don’t recognize the images above or if you prefer a physical copy, contact your doctor.
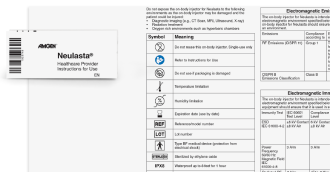
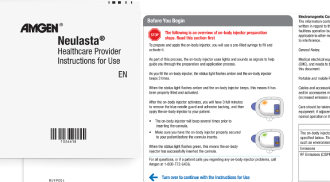
Onpro® Kit HCP Instructions for Use:
Which version of the Instructions for Use came with your patient's on-body injector?
Indication
Neulasta® (pegfilgrastim) is a prescription medicine used to help reduce the... Read More
Neulasta® (pegfilgrastim) is a prescription medicine used to help reduce the chance of infection due to a low white blood cell count, in people with certain types of cancer (non‑myeloid), who receive anti-cancer medicines (chemotherapy) that can cause fever and low white blood cell count.